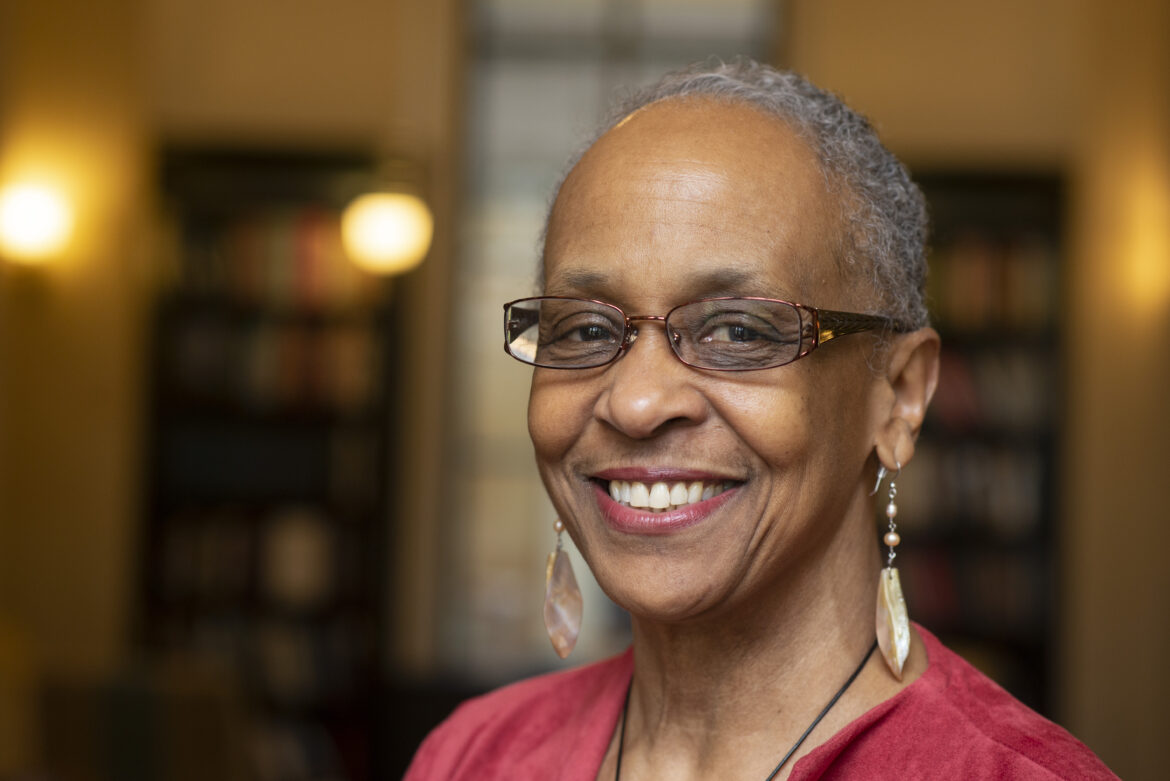
Dr. Shiriki Kumanyika is a research professor of community health and prevention at Drexel University’s Dornsife School of Public Health and emeritus professor of epidemiology at the University of Pennsylvania. Dr. Kumanyika’s expertise is in public health nutrition and strategies for achieving equity in the prevention and management of obesity and other diet-related chronic diseases. Her research during the past decade has focused on the racialized targeted marketing of unhealthy foods and beverages to Black children and adults. Dr. Kumanyika was the Founding Chair of the Council on Black Health, formerly the African American Collaborative Obesity Research Network (AACORN), which is now hosted by the Dornsife School of Public Health. The Council is a national organization with members in several U.S. states and a mission to create healthy Black communities. Dr. Kumanyika chairs the Food and Nutrition Board at the National Academy of Medicine and the Nutrition Guidance Expert Advisory Group for the World Health Organization. She is a past president of the American Public Health Association.
Food Policy Center: Thank you for agreeing to participate in this interview, Dr. Kumanyika. I’d like to start by asking how you initially became interested in food systems? You have a background in social work and the liberal arts – what drew you to nutrition and food justice?
SK: That is a bit of a long and winding road. My nutrition career started at Cornell University, almost accidentally. I was there in the early ‘70s as a spouse with my then husband, who had been a civil rights activist in New York City. We came to Cornell for him to study poultry science for future work in Africa. This was shortly after our return from a sponsored goodwill visit to six African countries. That was the time of the Pan African movement, when many Black Americans had ideas about connecting to the motherland, and my initial interest in nutrition focused on the possibility of working in Africa. I decided to take advantage of the Cornell environment studying something that would be useful for work in Africa. Since I already had a master’s degree in social work, I applied and was accepted into Cornell’s PhD program in nutrition (which meant that I had to take some extra science requirements right away). I was initially not aware that Cornell had one of the top nutrition science programs in the US and that I would be exposed to a very broad understanding of what “doing good” through nutrition could mean. A course taught by Daphne Roe, a British physician trained in social medicine, convinced me that public health nutrition was my future professional path – working at the intersection of nutrition with social and health problems. My dissertation focused on salt intake and high blood pressure. I knew, from helping out in my father’s medical practice in a Black community, that hypertension was a big problem in Black communities and that “cut out the salt” was even then standard advice.
After earning my PhD, I was recruited to join the Cornell faculty as an assistant professor assigned to teach the course in Community Nutrition whose subject matter at that time focused on the revelation that there was “hunger in America” (not only overseas) and looking at the relationships among poverty, poor nutrition, diet related diseases, and federal nutrition assistance programs such as the former Food Stamp Program and the supplemental Nutrition Assistance Program for Women, Infants and Children (WIC). The more I understood community nutrition, the more I realized that I wanted more formal training in public health and specifically epidemiology. I enrolled in the MPH program at Johns Hopkins, took all of my electives in epidemiology, and then remained there as a member of the faculty.
FPC: Much of your research has focused on policies and other programming to prevent obesity in the Black community. Why obesity? What particularly interests you about obesity as opposed to other diet-related diseases? (I recognize that you have done research on other diseases and disease states, but obesity stands out as a particularly salient topic for you.) What are the particular issues related to obesity that impact the Black community? How and why are those issues different from those that impact other communities?
SK: While I was searching for an anchor point for my research program at Hopkins, I learned that the above=average prevalence of obesity among Black women was an important but apparently also controversial issue. The controversies were whether this was actually true as opposed to an artifact of measurement or a “mammy” stereotype, and whether, if true, it was due primarily to Black/White genetic differences. These were compelling and understudied issues begging for solutions. Obesity-related conditions such as high blood pressure and type 2 diabetes affect an above-average percentage of the Black population, and these diseases may also be more severe, with more complications, in Black people. Once I concluded that the problem was real and not a genetic destiny, I became even more determined to find ways to address it. This was before public health data identified an epidemic of obesity and related health problems in the general population. The overall obesity epidemic made the importance of focusing on those most affected a mandate to try even harder to find solutions.
FPC: The Healthy Communities Study examined policies and programs that addressed childhood obesity in 130 U.S communities between 2010 and 2016. In a supplement overview published in Pediatric Obesity, you highlight the fact that the most effective strategies were those being employed in the Northeast and in high-income and White communities, but that community strategies were less likely to reach children in those demographic groups that are at the highest risk for obesity. Why is that, and what can be done to improve those outcomes?
SK: The same potential childhood-obesity prevention strategies were assessed in all the study communities. However, the specific strategies and combinations of strategies that were implemented varied in terms of which behaviors they focused on, their strength (the theoretical likelihood of their having an effect on behavior), and how long they were in place. According to the study authors, one likely explanation is that most were “universal,” that is, similarly applied without tailoring them to the particular situations of children or families in Black, Hispanic, or lower-income communities; better tailoring might have improved effectiveness. Also, there was less implementation of these strategies in the South and in African American communities, which might reflect availability of the resources needed to mount certain strategies. “Universal” strategies are likely to reflect approaches that have been found to work well in majority populations—the White and middle- or higher-income communities located in the Northeast. So the immediate answer about how to improve outcomes would be to focus on tailoring programs according to the evidence-based success of various design and implementation strategies. Analyses of the HCS database continue and may suggest specific potential strategies.
FPC: A growing body of research has highlighted the relationship between food insecurity and obesity. From your perspective, what role should obesity policies and programs play in addressing food insecurity?
Indeed, a paradoxical co-existence of obesity and food insecurity has been observed, for example, in food pantry clients with very low food security—paradoxical because obesity is generally associated with consuming too much food while food insecurity suggests the opposite. This may reflect the need to rely on inexpensive, high calorie-low nutrition foods that are easy to over consume—a problem that can be exacerbated if these are also the types of foods that are most available at food pantries. The policies that would help to address this problem are not necessarily “obesity policies and programs” but those related to the structures and practices of the charitable food system as well as the policies that determine access to federal emergency food, nutrition-assistance, and income-assistance programs. One core structural problem is the fact that the charitable food system was designed for emergencies or extraordinary circumstances that created food shortages during which any food would be good, so to speak. Some of these systems were also conceived before the current healthy diet recommendations were in place. Now, unfortunately, the food-banking system is a substantial food source for many people living in poverty or unstable economic circumstances. Policies and programs that adopt the principle of “nutrition security” will help to address this issue, i.e., looking at food security within the context of dietary quality and not just quantity. That principle is gaining increasing support, although major system changes are needed to realize this goal. Policies and programs that relate directly to obesity and management of other diet-related diseases can be connected to the charitable food system through strategic partnerships.
FPC: Can you talk a bit more about the degree to which you’ve found communities to be engaged in efforts to combat and prevent obesity? What kind of community outreach have you found to be effective for engaging historically underserved and marginalized communities in public health improvement initiatives?
SK: Unfortunately, I think we know more about the principles than about effective practices, and what we know may not always focus on food or obesity. From the Healthy Communities Study, we actually know that many of the recommended strategies work in populations that can make them work, presumably because the strategies were designed for those people and contexts. But we also know that these strategies are only theoretically effective in many communities that are substantially affected by obesity. A much smaller evidence base drawing on studies that have helped communities to leverage their own knowledge, institutional and network assets, and collective power has shown promising results—as, for example, many faith-based programs in Black communities. How do we generate more of these studies and practices? Communities of interest have many challenges and many priorities and focus on addressing these priorities. What we know about the principles points to authentic community engagement and ownership, embedding sustainability in stable existing programs or institutions. and equitable sharing of the available resources. It’s critical to understand and address power imbalances between those with the technical knowledge to implement programs and community leaders who can build the needed coalitions or networks to enable implementation.
FPC: You are leading Operation Good Food and Beverages (OGF&B) – a national youth counter-marketing campaign to promote healthier foods among Black youth. Can you speak a little bit about this campaign? What roles do technology and social media play in the marketing of food to young people? What are some of the challenges you’ve faced in launching OGF&B?
SK: Food and beverage advertising is a major influence on our eating patterns, but that influence is largely ignored or taken for granted in mainstream nutrition interventions. Most advertising is inconsistent with recommended dietary patterns in that it over-promotes products that are high in fat, sugar, and salt and low in dietary fiber and under-promotes healthier items. A minuscule amount of the billions spent on food advertising is devoted to the promotion of healthy foods and beverages. The most heavily promoted foods and beverages are those that contribute to weight problems, diabetes, and high blood pressure—problems that are critical health issues in Black communities.
We designed our campaign—OGF&B: “A Black Community Imperative”—to challenge the longstanding pattern of racialized food marketing, which results in a particularly unfavorable pattern of food marketing to Black communities. Exposure to ads for unhealthy foods may be two or three times higher for Black youth compared to their White counterparts. Food marketing generally relies on profits from products at the least healthy end of the spectrum and also directs promotions to people who are considered “likely customers.” Identifying the likely customers for the least healthy products on the basis of race unavoidably leverages broader race-related injustices in American society and contributes to health disparities.
OGF&B adds a Black consumer voice to the conversation about food marketing, thus challenging the proposition that there is no demand for healthier products in Black communities. We raise awareness of what we want to see (vs. don’t want to see) in terms of food promotions and food access in Black communities. We have a petition asking members of the National Restaurant Association to engage in a dialogue about how to extend the use of nutrition standards to main menu items rather than only kids meals.
The campaign has a website with key messages and other information related to “good food and beverages,” a link to the petition, and Instagram and TikTok accounts. Digital marketing, which has apparently become the major focus of advertising in the food sector, benefits from the ever-evolving modern techniques for using consumer data to personalize ads. The campaign is Black youth-inspired because of their especially high exposure to unhealthy food ads, and because youth advocacy can be very effective in reaching both youth and adult audiences. Young people are heavily immersed in and influenced by social media in various ways. Untoward effects on their food preferences and food consumption patterns are among the less favorable types of influence. Because of this, our campaign focuses on high school and college age youth.
We have had to cope with two main challenges. One is with the topic itself. The realities are that: 1) the marketing practices of large corporations enjoy the protections of free speech and are difficult to change through regulations and 2) the scale and power of commercial marketing are much greater than public health efforts, and 3) spurious arguments grounded in the concept that anything wrong in the free marketplace will be self-correcting, and 4) the current marketing practices are legal, leaving healthy food advocates to appeal for equity in the balance of foods marketed to racial/ethnic groups or low-income communities on moral grounds—and even these arguments are not readily agreed on among ethicists. OGF&B attempts to catalyze a movement that can help to alter food marketers’ perceptions of Black consumers’ demand for healthy foods.
The other key challenge has been the need to resist or suppress the tendency to sensationalize the striking nature of the facts involved—the money spent on marketing of unhealthy vs. healthier foods and beverages, the Black/White disparities in exposure and diet-related health problems. The idea that pointing out disparities can compel changes in the industry may seem reasonable, but to date only minor changes and concessions related mostly to children’s ad exposures have occurred.
FPC: Have there been people or groups that were skeptical or unwilling to get on board?
SK: Response to the campaign has been very favorable. Even potential skeptics who favor bolder, more direct approaches to influencing food industry behavior seem to see our campaign as adding a refreshing element to the conversation.
FPC: Did you have any difficulties determining the best ways to connect with the communities and populations you are targeting?
SK: Yes—the need to rely on virtual interactions. Most of the key contributors to the development of the campaign have never met in person, and many local community activities that would have facilitated dissemination could not take place because of COVID precautions.
FPC: How can interested organizations get involved?
SK: Interested organizations can rally around our efforts to work with the National Restaurant Association or others to improve main menu items or food items that would be popular with Black teens by getting their members to visit the OGF&B website, click on “Add your Name,” and sign our chage.org petition. They can also contact the Council on Black Health at info@councilbh.org to sign up for the next phase of campaign dissemination, which is currently in the planning stages.
FPC: What is the one food policy change at the federal level that could have the greatest impact on hunger?
SK: Apologies in advance here. I tend to resist questions about the “one best thing” when it relates to a longstanding and complex systems problem like food insecurity in the United States, because no one change could topple the mountain of problems we have in this arena. The US has no business having anything even remotely like hunger except in unusual or extreme circumstances. I would argue that the same thing goes for any level of food insecurity. From this perspective, my answer is that, to end hunger the policy would not be about food as such but about doing the rejigging of the aspects of society that are necessary to make sure that all Americans can routinely meet their basic needs through conventional channels. These channels would, of course, include provisions for people who need assistance in the face of disability, emergencies, or other temporary untoward circumstances.
I see the current food insecurity situation as a structural problem, not just in the structure of charitable food systems or food banks but also more fundamentally in the failures of our core social and economic systems. In times such as the COVID-19 pandemic, we see an outpouring of charity from many, many corners—companies, celebrities, and communities—but we have to ask ourselves why it is only in such situations that people have empathy for those with limited economic resources and power to meet their needs? Many of the people most seriously affected by COVID-19 can be described by demographic characteristics such as race that the average person recognizes and accepts as being associated with social disadvantage. Is it only when the evidence that poverty and limited power are not matters of personal responsibility that it becomes overwhelmingly undeniable that it is important to help those in need? I hope the structural issues that foster and perpetuate chronic poverty and marginal existence for so many people in this country will receive a lot more consideration going forward. Perhaps the upcoming White House Conference on Hunger, Nutrition and Health will become the tipping point for deeper thinking on these issues.
From a practical perspective, I think the question you are asking is what would have the greatest impact today and in the near future. My answer is to focus heavily on the design and implementation of a well-coordinated, integrated, systems-oriented nutrition safety net based on optimizing the available nutrition assistance programs and creating new ones to close gaps in coverage and streamline access. The systems-oriented part is because people and societies change, and because climate change will increasingly create challenges that need to be anticipated.
FPC: What was your proudest food advocacy moment?
SK: Early in the first Obama administration, I had the privilege of being in a group of experts periodically called on to advise the First Lady about initiatives she might undertake. Having a chance to speak and be one of two people chosen to lead a small invited briefing session with Mrs. Obama was transformative for me—speaking to power at that level. The Let’s Move initiative included strategies that were consistent with the key recommendation I made at that time. I am sure that many other advocates made similar recommendations, but I was, and still am, very proud to have been a part of that conversation.
Fact Sheet
Where you grew up: Baltimore, Maryland
Where you call home: Philadelphia, Pennsylvania
Job title: Research Professor in Community Health and Prevention, Drexel University Dornsife School of Public Health and Emeritus Professor of Epidemiology, University of Pennsylvania
Background and education: Public schools in Baltimore Maryland; undergrad in psychology at Syracuse University; Master of Science in Social Work from Columbia; PhD in Nutrition from Cornell University; Master of Public Health from Johns Hopkins
One word you would use to describe our food economy: Misguided
Your food policy hero: Michelle Obama, for the reasons I stated above and for what came out of Let’s Move.
Your breakfast this morning: coffee, bran cereal and fruit with water (I only like milk in coffee), and an egg
Favorite food: Kale
Favorite last meal: Whole wheat spaghetti with red clam sauce